You may have heard the term vagus nerve in the gut health realm but what is it and what exactly is the connection between the vagus nerve and IBS or SIBO?
As a gut health Registered Dietitian who has seen hundreds of clients overcome IBS and SIBO, I am almost always incorporating nervous system regulation and more specifically vagus nerve stimulation into my clients protocols. In this blog, I will review what the vagus nerve is, the connection between the vagus nerve and IBS and SIBO, and ways to strengthen your vagus nerve.

What is the Vagus Nerve?
The Vagus Nerve is one of twelve cranial nerves in your body. It is actually our longest nerve, running from the brain all the way down to your abdomen, connecting a number of other organs along the way. (1)
The vagus nerve is part of the autonomic nervous system (ANS), which controls all the automatic systems in the body. The ANS is comprised of the parasympathetic nervous system (PNS) and the sympathetic nervous system (SNS).
The PNS is a system of nerves that is responsible for the “rest and digest” response, or in other words, the state of relaxation, rest, and digestion. Alternatively, the SNS is the response to stress known as the “fight or flight” response. While the SNS is crucial for being able to react when our body is in a state of threat, it is important that our bodies are balanced and able to shift back to the PNS the majority of the time.
Functions of the Vagus Nerve
The vagus nerve is a key component of the parasympathetic nervous system (PNS) and helping maintain homeostasis in the body. It is essentially the switch that turns on communication from the brain to the various organs. Below are some of the main functions of the vagus nerve as it relates to IBS.
Regulates Digestion
The vagus nerve plays a huge role in multiple steps of your digestion. Digestion starts the moment food hits your mouth. This is where the vagus nerve first makes it’s appearance. It stimulates the production of stomach acid (hydrochloric acid (HCL)) via the neurotransmitter acetylcholine. Stomach acid or HCL is crucial for breaking food down and neutralizing harmful bacteria. (2)
The vagus nerve also controls gastric motility. When your vagus nerve is stimulated, it turns on and coordinates the migrating motor complex (MMC). The MMC is the housekeeper of your gut. It is a series of waves of contractions in your gut that takes place in a fasting state. During this state, undigested food and bacteria are swept through the small intestine and into the large intestines. (2)
Lastly, the vagus nerve controls your hunger and satiety cues. When you are hungry, your body produces hunger hormones known as ghrelin. In comparison, when your stomach is empty, ghrelin gives you the signal to eat. When you are full, your leptin hormone comes in to play. The vagus nerve is an integral component for these hormones to work effectively. (3)
Supports the Immune System
The vagus nerve also influences your immune response through the cholinergic anti-inflammatory pathway. In this pathway, the vagus nerve releases acetylcholine which binds to immune cells or macrophages, reducing the production of pro-inflammatory cytokines. This in turn helps suppress excessive inflammation which reduces excessive immune responses. This can improve the body’s response to infections and other chronic conditions. Research suggests stimulating your vagus nerve can treat inflammation and lower chances of developing infection and autoimmune conditions. (4)
Modulates Heart Rate and Regulates Breathing
As mentioned earlier, the vagus nerve is a main component of the parasympathetic system or in other words the “rest and digest” state. When your body undergoes stress, your “fight or flight” system is stimulated. The vagus nerve helps regulate heart rate, slowing it down to transition from fight or flight to rest and digest. Stimulating your vagal tone has been linked to improvement in your ability to adapt to stress. (5)
The vagus nerve is also involved in the respiratory system. It is involved in regulating the rhythm of breathing by sending signals to the diaphragm and other respiratory muscles. It also is able to adjust the airways diameter depending on the body’s needs. For example, when you are working out, the body will signal the body to expand the lungs as opposed to when you are at rest when your breathing rate is slower. (5)
Vagus Nerve: Role in the Gut-Brain Axis
The vagus nerve is the nerve that connects the brain and the gut. This connection is the gut-brain axis and is a bidirectional communication between the gut and the brain. It sends signals from the brain to your gut and visa versa. (6)
Gut to Brain Communication
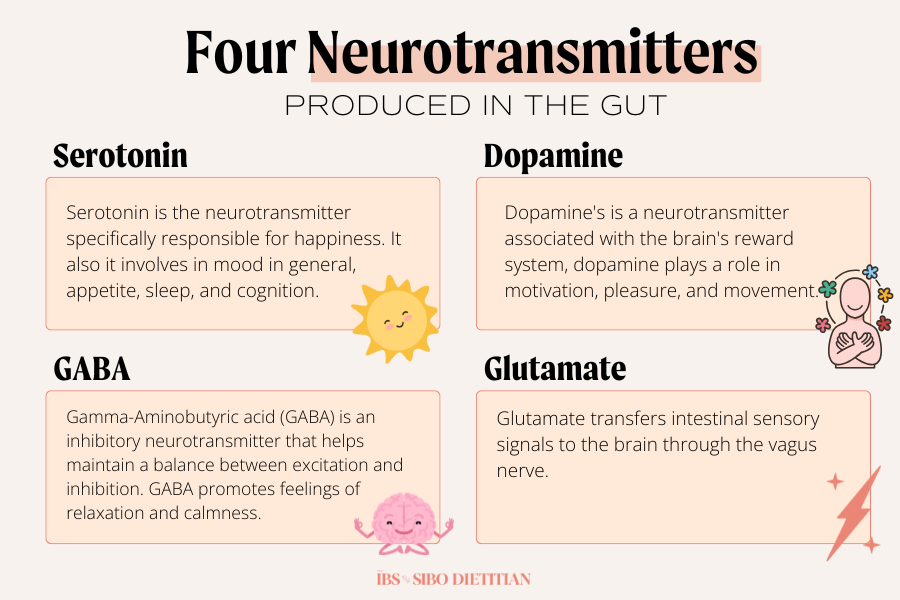
The connection of the brain and the gut starts in the microbiome. When you consume a wide variety of fibers and prebiotics, this provides the microbes fuel. The microbes metabolize the fuel, turning it into byproducts such as short chain fatty acids (SCFA) and neurotransmitters, specifically serotonin, GABA, dopamine, and glutamate. The vagus nerve is responsible for transporting these neurotransmitters across the blood-brain barrier to influence mood, anxiety, stress, and even memory. (6)
Brain to Gut Communication
While your gut is busy producing neurotransmitters to send to your brain, your brain is hopping on the two-way high way to your gut. Your brain sends signals to your gut to start digesting food with even the thought of consuming food. The signals being sent from your brain to your gut can control hunger, satiety, digestion, and even motility. (6)
Vagus Nerve and IBS Connection
What is IBS?
Irritable Bowel Syndrome (IBS) is a gastrointestinal disorder that displays with symptoms of bloating, abnormal bowel habits, abdominal pain, and gas. It is a functional disorder that is diagnosed based on exclusion. This means that it is not something that can be detected by scopes or labs and but rather diagnosed by presentation of symptoms with other conditions such as celiac disease, crohn’s, and colitis being ruled out. While the cause of one developing IBS is still not fully understood, it is suggested that one mechanism is a disruption in the gut and brain connection.
Vagal Tone and IBS
Those with IBS often deal with lowered or dysregulated vagal tone. (7) Vagal tone refers to the amount of activity of the vagus nerve. Low vagal tone in IBS can lead to:
- Motility issues – Low vagal tone effect the Migrating Motor Complex (MMC) leading to slower motility (constipation) and spastic peristalsis (diarrhea).
- Visceral Hypersensitivity – The poor vagal tone weakens the brains ability to coordinate and regulate pain signals from the gut effectively. This can heighten the perception of pain and discomfort.
- Stress – While stress can be a driver of low vagal tone, the dysfunction of the communication of the brain and the gut can lead to a vicious chicken or the egg situation where stress can cause symptoms and vice versa
How to Support the Vagus Nerve for IBS Relief
If you believe you may have low vagal tone, it is reversable. There are many ways that you can support your vagal tone by stimulating your vagus nerve including change in diet, simple lifestyle changes, and even exercise and/or therapy.
Nutrition and the Vagus Nerve
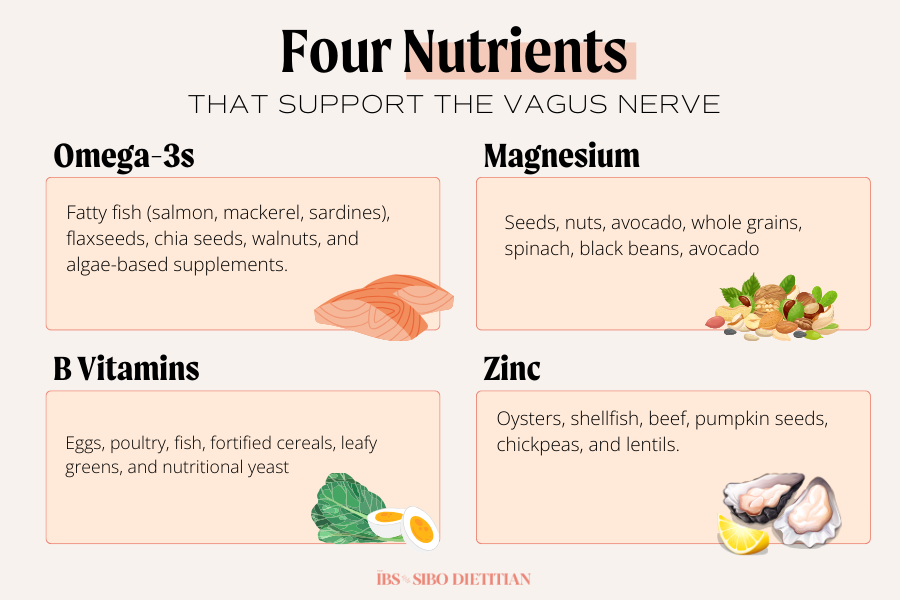
- Omega 3s – They improve vagus nerve tone by reducing inflammation and enhancing communication between the brain and gut. You can find omega 3s in fatty fish (salmon, mackerel, sardines), flaxseed, chia seeds, walnuts, and algae-based supplements.
- Magnesium – Magnesium is essential for nerve function and plays a role in activating the parasympathetic nervous system, including the vagus nerve. Foods rich in magnesium include seeds, nuts, avocado, whole grains, spinach, black beans, and avocado.
- B Vitamins – They are essential for vagus nerve support because they facilitate neurotransmitter synthesis, support nerve protection (B12), and ensure efficient vagal signaling. If you are trying to add more B Vitamins, they can be found in eggs, poultry, fish, fortified cereals, leafy greens, and nutritional yeast.
- Zinc – Zinc is essential for maintaining your parasympathetic nervous system and promoting overall vagal tone. To get zinc from your diet, you would want to add oysters, shellfish, beef, pumpkin seeds, chickpeas, and lentils.
Lifestyle Strategies
- Deep Breathing Exercises – You can easily perform diaphragmatic breathing or belly breathing in any setting. It is performed by slowly inhaling through your nose, contracting your diaphragm (pulling in your stomach) and exhaling slowly through your mouth, relaxing your diaphragm (pushing out your stomach). This triggers your relaxation response and improves vagal tone.
- Meditation and Stress Reduction – Meditation can increase vagal tone, which can help you regulate stress responses. Furthermore, it improves your mood and puts you in a relaxed state, while simultaneously strengthening the vagal tone.
- Cold Exposure– Splashing cold water on your face or taking a cold shower can wake up your vagus nerve. When we’re exposed to the cold, our fight or flight mode gets suppressed, switching on our rest and digest.
- Humming/Singing – Your vagus nerve runs by your vocal cord. This means humming or even singing causes vibrations that stimulate the vagus nerve. Gargling water in the morning can also be a way to send vibrations to your vagus nerve.
Therapies for Vagus Nerve Stimulation
- Nerve Stimulation devices – Nerve stimulating devices can be surgically placed or you can purhcase a non-invasive option. It is essentially a pacemaker for your brain, sending electrical signals to the vagus nerve.
- Acupuncture – Acupuncture is a traditional Chinese Medicine practice where needles are inserted in the skin at certain parts of the body. Studies show that acupunture can be a less expensive and safe substitution to implanted devices (8)
- Gut Directed Hypnotherapy – Gut directed hypnotherapy can be done in person or via apps such as the Nerva app. This type of therapy fixes the miscommunication between your brain and your gut, strengthening your vagus nerve and thus improving IBS symptoms.